We all have seen patients who have macular edema or other retinal pathology that is obvious both on retinal examination and OCT interpretation. Other conditions, such as hydroxychloroquine (Plaquenil) retinal toxicity, can present in a much more subtle fashion, which is why the use of ancillary testing that examines both structure and function is so critical. Hydroxychloroquine toxicity is a rare condition, but all eye care practitioners need to be aware of the proper screening and examination guidelines for
numerous reasons:
- The likelihood of toxicity increases the longer a patient is on the medication.
- We all see hydroxychloroquine patients on a regular basis.
- Once damage is present it is typically not reversible and, because hydroxychloroquine is cleared slowly from the body, further damage can occur even after cessation of the drug.
Risk factors for the development of hydroxychloroquine retinal toxicity include pre-existing retinal or macular disease, kidney dysfunction, daily dose of hydroxychloroquine > 5.0 mg/kg/day, and a total cumulative dose of hydroxychloroquine > 1000 g. How long does it take for a patient to get to 1000 g total cumulative dose? It depends on the daily dose. In our clinic, most patients take 200 mg tablets twice daily (400 mg daily). At that dose, the patient will reach the 1000 g threshold in about seven years. If a patient takes 200 mg daily, they will double that timeframe to approximately 14 years.
The risk of toxicity before that cumulative dose is reached (before five to seven years of use) is almost negligible, but it increases to about 1% after that time once the 1000 g total cumulative dosage has been reached. The risk continues to increase the longer patients are on the medication and the more
the cumulative dose accumulates. Based on the assumption that screening is justified as the risk of toxicity approaches 1%, annual screening should be performed on all patients who exceed five
to seven years of exposure at 400 mg daily. However, earlier, more frequent screening may be indicated where there are unusual risk factors or a suspicion of early toxicity.
On OCT, it is important for eye care providers to take a close look at a macular cube scan or high-definition raster scan through the central and paracentral macular area. Pay close attention to
the outer retinal layers, particularly in the parafoveal area. Any dropout or loss of the photoreceptor integrity line (PIL), which represents the junction of the inner and outer photoreceptor segments, indicates possible early hydroxychloroquine toxicity.
This effect can begin subtly (see Figure 1) and become much more obvious as the condition progresses. With atrophy of the outer retina and PIL on each side of the fovea, it can give the
appearance of a “flying saucer” or “UFO” sign (see Figure 2).
Early detection is critical to prevent further progression of the disease, with the current line of thinking that mfERG, OCT or fundus autofluoresence will likely detect early hydroxychloroquine toxicity before fundus examination and even visual field in most cases. Utilizing functional and structural tests together, such as 10-2 VF and OCT testing, will likely yield the best diagnostic value.
As OCT technology evolved over the last 10 to 20 years, it has allowed us to see structures and layers of the retina that we couldn’t evaluate before. These developments have allowed earlier diagnosis, more timely management and better long-term outcomes for our patients.
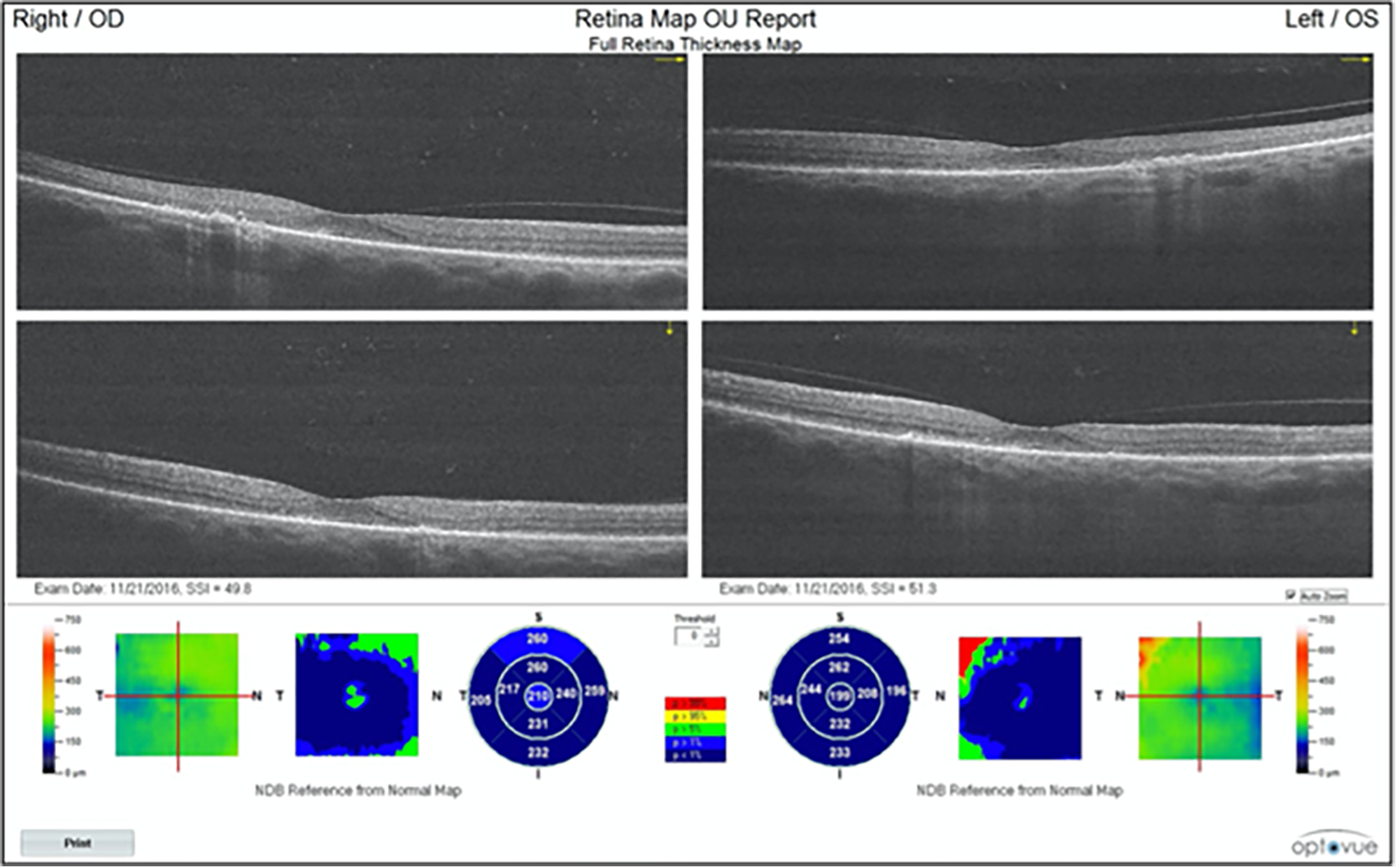 Figure 1. This Optovue OCT shows disruption of the outer retina with disappearance of the PIL on either side of the fovea.
Figure 1. This Optovue OCT shows disruption of the outer retina with disappearance of the PIL on either side of the fovea.
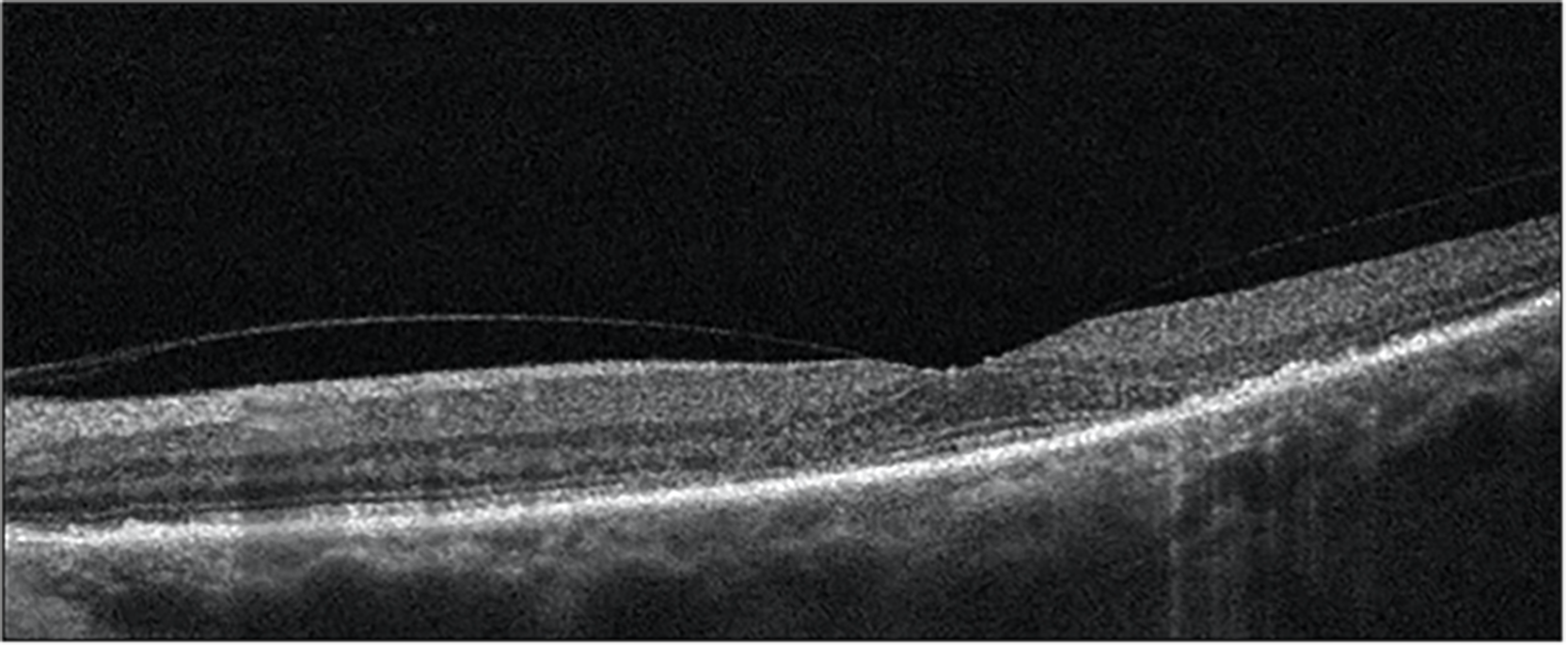 Figure 2. This Optovue OCT shows the classic saucer sign appearance. PIL is still intact underneath the fovea, with atrophic changes seen on both sides of the fovea.
Figure 2. This Optovue OCT shows the classic saucer sign appearance. PIL is still intact underneath the fovea, with atrophic changes seen on both sides of the fovea.

Nate Lighthizer, OD, FAAO
Born and raised in Bismarck, ND, Nate Lighthizer, OD, FAAO, is a graduate of Pacific University College of Optometry. Upon graduation, he completed a residency in Family Practice Optometry with an emphasis in Ocular Disease through Northeastern State University Oklahoma College of Optometry. Dr. Lighthizer has since joined the faculty at the Oklahoma College of Optometry and serves as the Chief of Specialty Care Clinics and the Chief of Electrodiagnostics Clinic. In 2014, he founded and now heads the Dry Eye Clinic at the College of Optometry. Also in 2014, he was named the Director of Continuing Education as well as the Assistant Dean for Clinical Care Services at the Oklahoma College of Optometry. He is a founding member, and currently serves as Vice President, of the Intrepid Eye Society which is a group of emerging thought leaders in optometry. He was named a member of PCON 250—a list of the top 250 optometrists in the country who practice progressively, provide innovative patient care, conduct optometric research or excel in academia and share what they have learned with other optometrists to advance the profession. Dr. Lighthizer lectures nationally on numerous topics, most notably advanced ophthalmic procedures, electrodiagnostics and ocular disease.
The information is intended for general informational purposes only. It is not intended as, and should not be considered, a substitute for professional medical advice, diagnosis, or treatment.
The content is not designed to replace the relationship that exists between a patient and their healthcare provider. Any medical decisions should be made in consultation with a qualified healthcare professional who can provide information tailored to your individual circumstances.
Medical procedures, case studies, and practices mentioned in this content may vary based on regional standards, local regulations, and the discretion of the providing healthcare professional. What may be considered appropriate and ethical in one country may differ in another.
The content may include general references to medical practices, medications, or treatments that are widely accepted in certain regions but may not be applicable or endorsed universally. It is important to consult with a healthcare professional in your jurisdiction to ensure the information is relevant to your specific situation.
The authors, publishers, and contributors of this content disclaim any liability for any adverse effects resulting directly or indirectly from information contained in this content. Readers should exercise their own judgment and seek the advice of healthcare professionals as appropriate.
By accessing and using this content, you acknowledge and agree to the terms of this disclaimer.
![[OCT Article] The Subtle Things Matter When It Comes to Certain Retinal Conditions Image](https://blog.visionix.com/hs-fs/hubfs/2-Oct-17-2023-10-11-10-8581-AM.png?width=1250&name=2-Oct-17-2023-10-11-10-8581-AM.png)