[OCT Article] Advanced Diagnostics Help Advanced Treatments
As our technologies evolve, we begin to understand how they can be utilized to care for some of more advanced cases. Here is an example of how advances in OCT are being leveraged to better care for patients.
![[OCT Article] Advanced Diagnostics Help Advanced Treatments Image](https://blog.visionix.com/hs-fs/hubfs/Figure%203.%20Picture%20of%20the%20patients%20left%20eye%20the%20following%20day..png?width=1250&name=Figure%203.%20Picture%20of%20the%20patients%20left%20eye%20the%20following%20day..png)
- A 31 year old female came in to the office for an emergency visit. One hour before she came to the office she heard a pop come from her left eye and her vision became very blurry. She was wearing her contact lenses at the time. She removed her lens because she thought the pop was from her contact. Her eye became sore with her lens on her eye. She removed the lens and her eye was still very sore.
The patient has approximately 4.00 diopters of regular astigmatism at axis 180 in both eyes. We saw her previously and ruled out keratoconus. Entering vision at todays visit with the left eye wearing her glasses was 20/100 (previously was correctable to 20/20). Her intraocular pressure was 16mmHg. Her cornea was remarkable for severe corneal edema (figure 1).
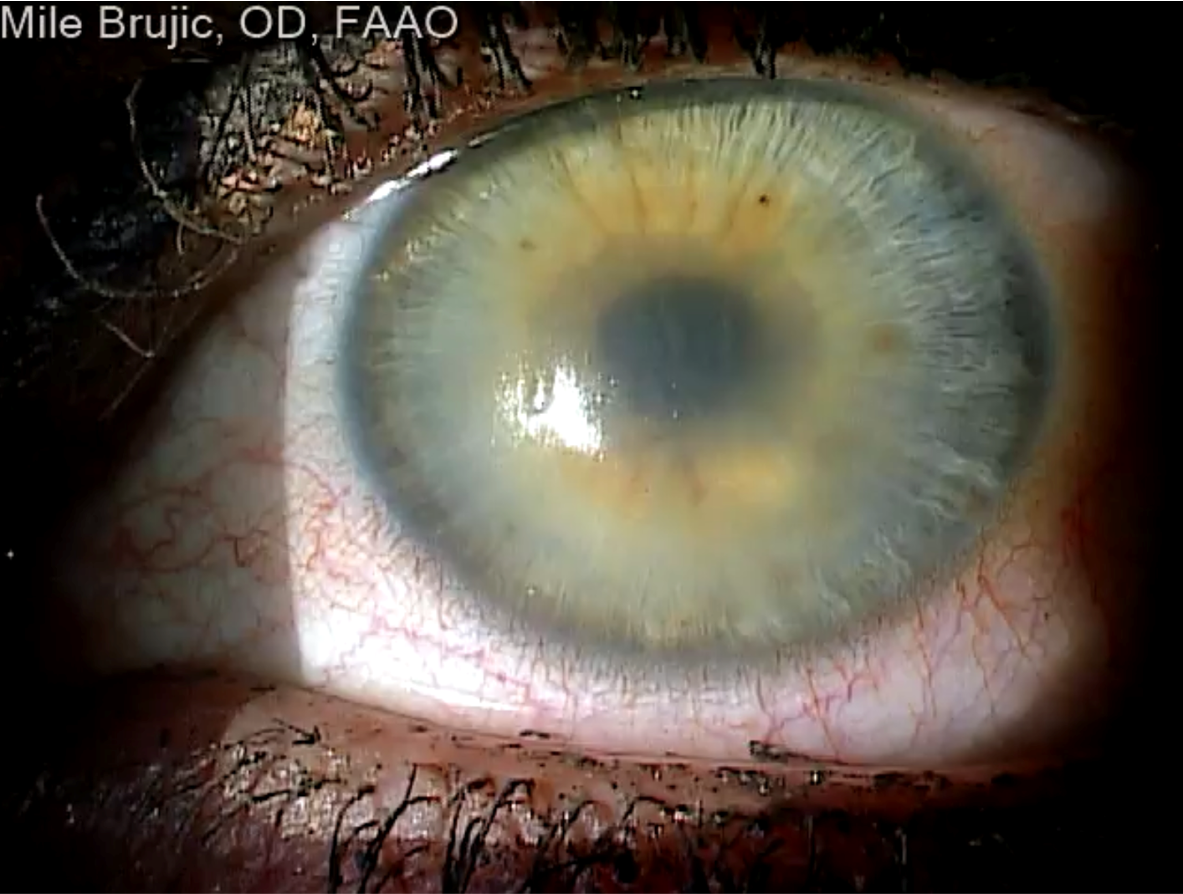
Figure 1. Significant corneal edema.
A peculiar small well delineated region was seen inferiorly on the corneal surface (figure 2). Anterior segment OCT scans were ordered and demonstrated substantial corneal swelling (figure 2). Additionally, a small region of an epithelial detachment was noted in the small delineated region when viewed with the OCT cross section (figure 2).
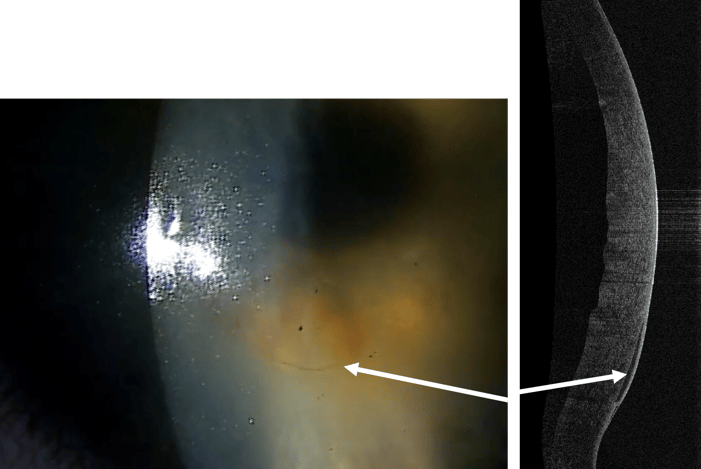
Figure 2. Small delineated region on the anterior cornea noted as an epithelial detachment on OCT cross section.
The unclear clinical picture made a definitive diagnosis difficult. I wondered if something may have inadvertently hit her in the eye (over the contact lens) creating the popping sound and resulting in the corneal edema. The patient was prescribed prednisolone acetate 1% drops every 30 minutes for 4 hours then every hour until she went to bed that evening. She was to continue 1 gtt every hour the following day until she was seen in the office.
When she came into the office, she reported a significant improvement in vision and her eye felt back to normal. Vision with her left eye was 20/20. Her corneal edema had significantly improved as seen on the external photo taken by the OCT (figure 3).
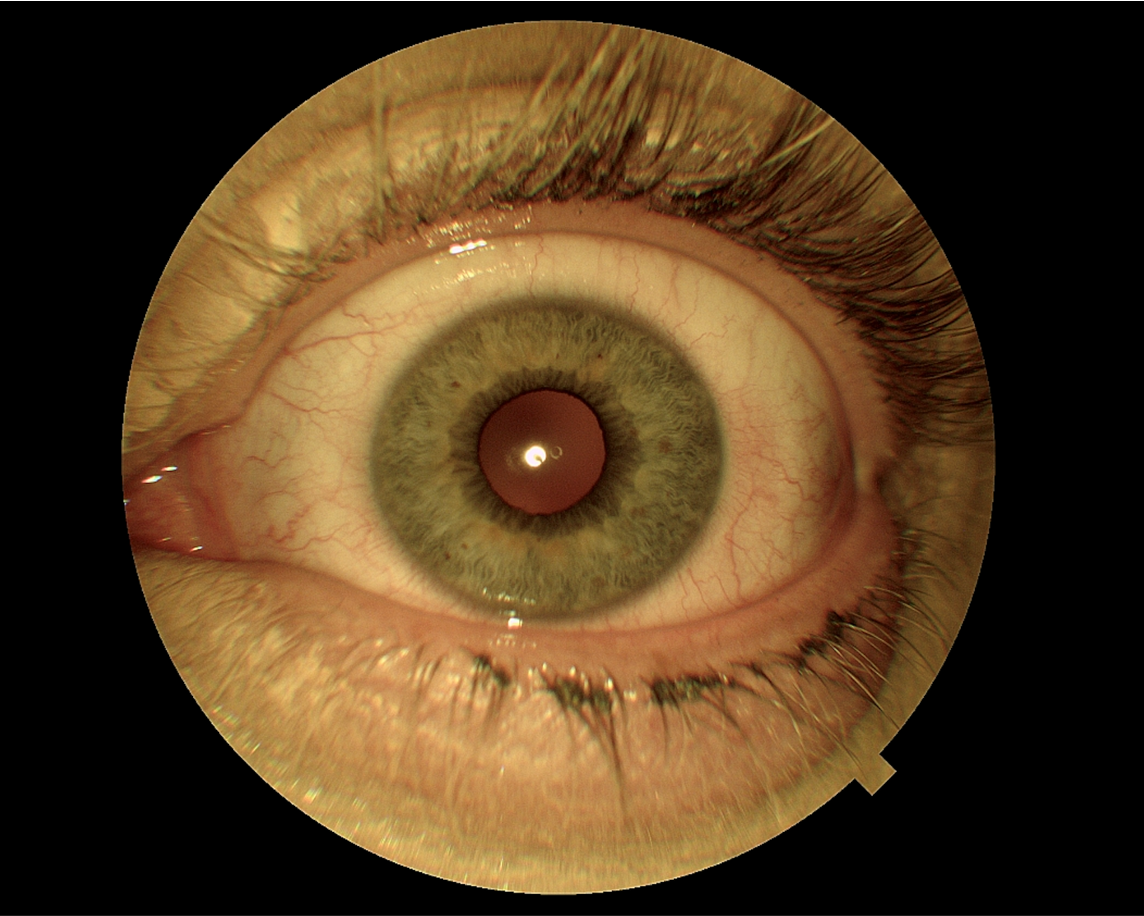
Figure 3. Picture of the patients left eye the following day.
There was a significant improvement in corneal edema as measured by the corneal map functionality (figure 4).
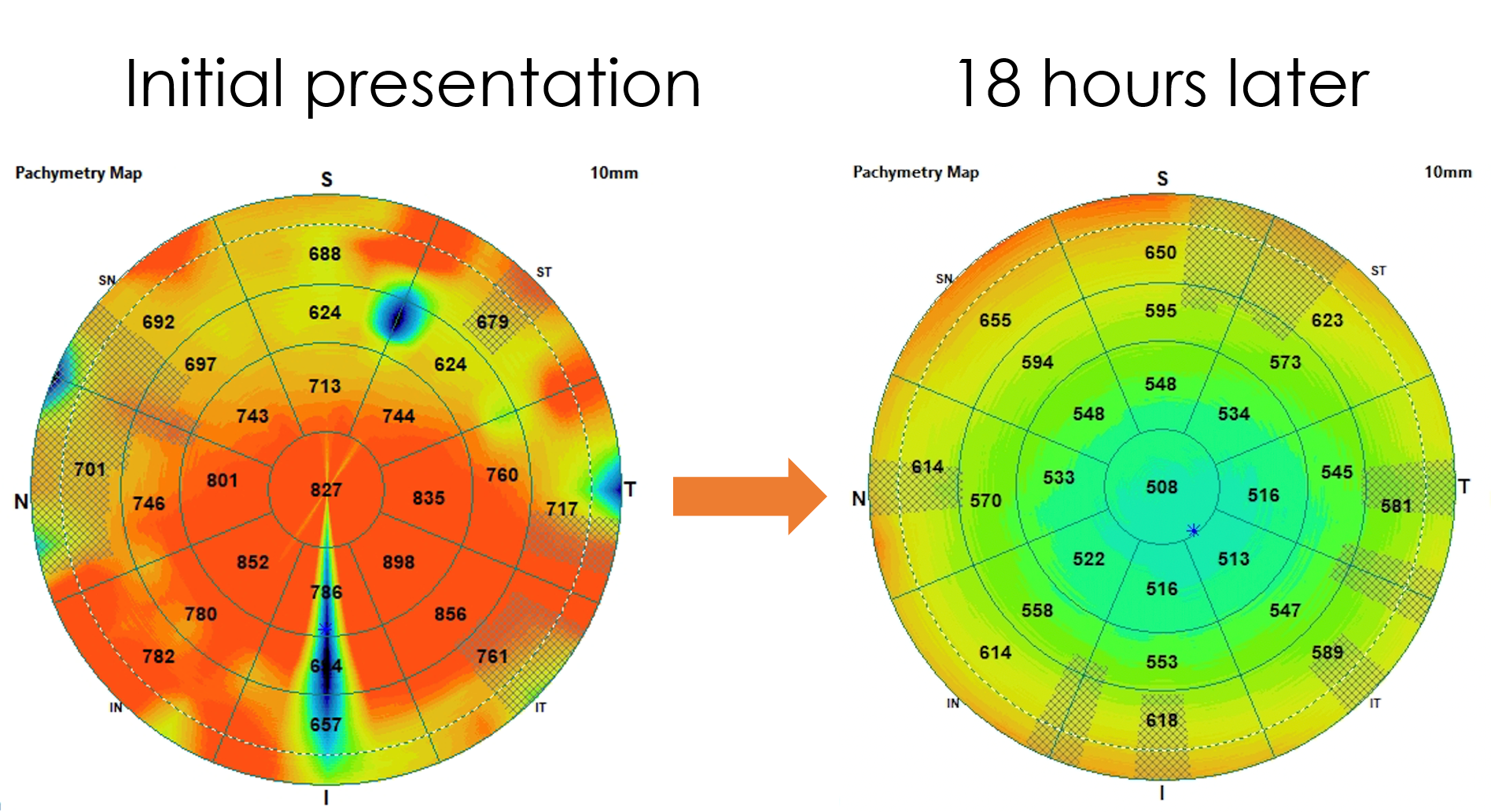
Figure 4. Pachymetry scan at initial presentation and the following day. Note the significant improvement in edema.
When the corneal cross section from the day before is compared to today’s measurement, the epithelial detachment had also resolved (figure 5).
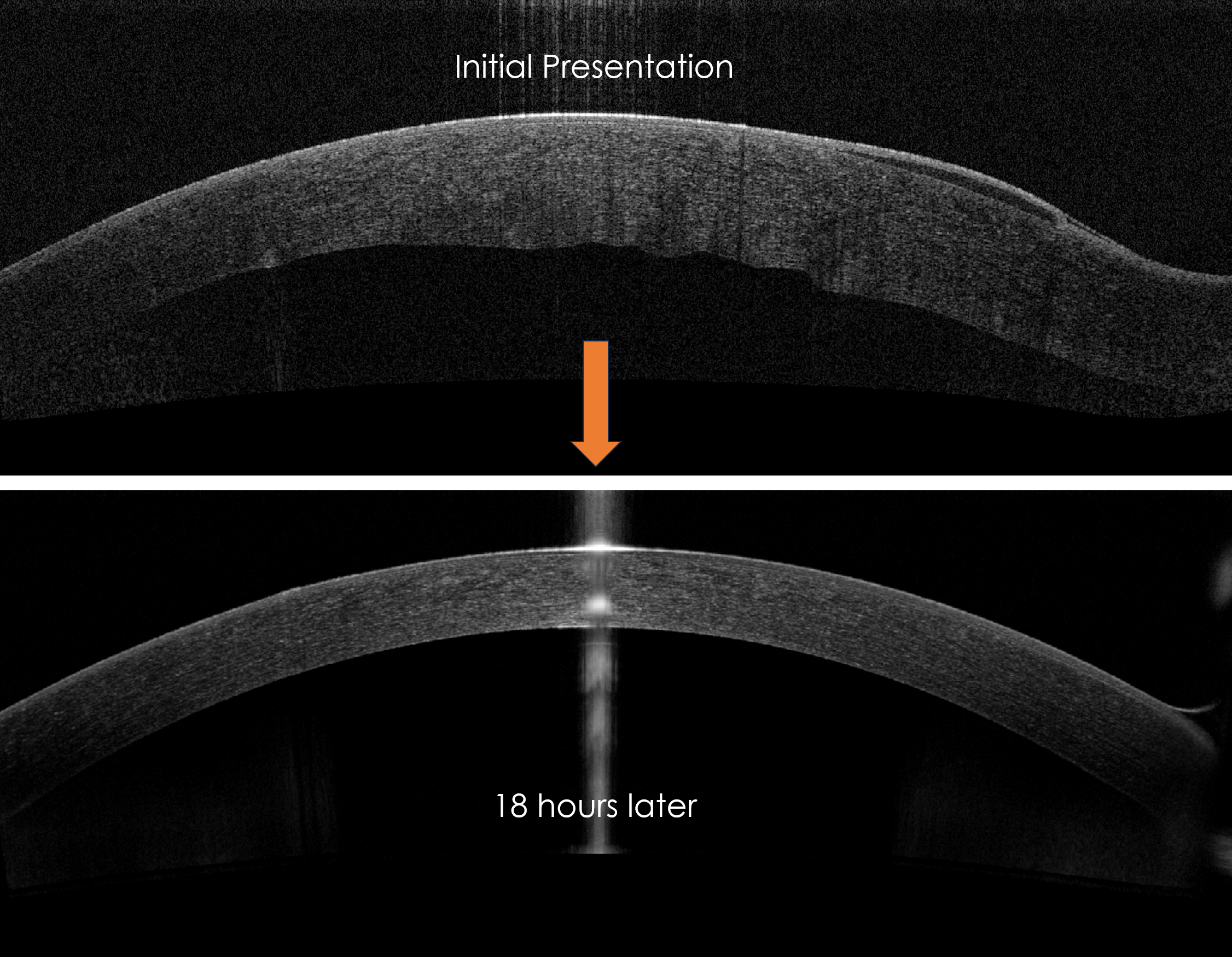 Figure 5. OCT of initial presentation and the following day.
Figure 5. OCT of initial presentation and the following day.
- The patient was asked to use corticosteroid eye drop four times the day of the follow up and to reduce the number of drops one a day until she was done with the drops. I followed up with the patient a week later with continued resolution of symptoms. This is an example of advanced technologies assisting with optimizing advanced treatments.
Mile Brujic, OD, FAAO is a 2002 graduate of the New England College of Optometry. He is a partner of Premier Vision Group, a successful four location optometric practice in Northwest Ohio. He practices full scope optometry with an emphasis on ocular disease management of the anterior
segment and specialty contact lenses. He is active at all levels of organized optometry. Dr. Brujic is on the editorial board for a number of optometric publications. He has published over 450 articles and has given over 2000 lectures, both nationally and internationally on contemporary topics in eye care. He was elected Young Optometrist of the Year (2011-2012) and among the 50 most influential optometrists by Optometric Management in 2015
The information is intended for general informational purposes only. It is not intended as, and should not be considered, a substitute for professional medical advice, diagnosis, or treatment.
The content is not designed to replace the relationship that exists between a patient and their healthcare provider. Any medical decisions should be made in consultation with a qualified healthcare professional who can provide information tailored to your individual circumstances.
Medical procedures, case studies, and practices mentioned in this content may vary based on regional standards, local regulations, and the discretion of the providing healthcare professional. What may be considered appropriate and ethical in one country may differ in another.
The content may include general references to medical practices, medications, or treatments that are widely accepted in certain regions but may not be applicable or endorsed universally. It is important to consult with a healthcare professional in your jurisdiction to ensure the information is relevant to your specific situation.
The authors, publishers, and contributors of this content disclaim any liability for any adverse effects resulting directly or indirectly from information contained in this content. Readers should exercise their own judgment and seek the advice of healthcare professionals as appropriate.
By accessing and using this content, you acknowledge and agree to the terms of this disclaimer.