[OCT Observations] Utilizing Full-Range Anterior Chamber Scans in the Management of Glaucoma
Optical coherence tomography (OCT) has been used by clinicians for several years as an adjunct to gonioscopy. While OCT angle imaging has been helpful with angle evaluation, its main limitation lies in the inability to see limbus to limbus. It is difficult to accurately assess angle structure without being able to visualize full iris configuration. Fortunately, recent advances in OCT technology allow us to image the whole anterior chamber.
![[OCT Observations] Utilizing Full-Range Anterior Chamber Scans in the Management of Glaucoma Image](https://blog.visionix.com/hs-fs/hubfs/Fig1abc.jpg?width=1250&name=Fig1abc.jpg)
While there are many clinical situations in which limbus to limbus imaging provides value, three pathologies areclarified by this type of OCT: primary angle closure suspects (PACS), pigment dispersion syndrome with reverse pupillary block and plateau iris syndrome.
Case 1: PACS
A 62-year-old Hispanic male with known narrow angles presented to the office for an exam. His refractive error was +2.00 OD and OS, and he had mild cataracts. His Van Herick was graded as a 2. Using the Ocular Response Analyzer, his intraocular pressure (IOP) measured 13.5 and 13.2. Gonioscopy showed greater than 180° of iridotrabecular contact with no peripheral anterior synechiae. Angle OCT confirmed narrow angles (Figure 1A). He had no evidence of glaucomatous optic neuropathy with unremarkable OCTs and fields, so we diagnosed him as a PACS. Due to the ominous appearance of his angle OCT, our surgeon promptly performed laser peripheral iridotomy OU, which opened the angle slightly (Figure 1B). During his six-month follow up, he complained of worsening night glare, and we proceeded to cataract surgery to further open his angle (Figure 1C). We are now following him yearly.
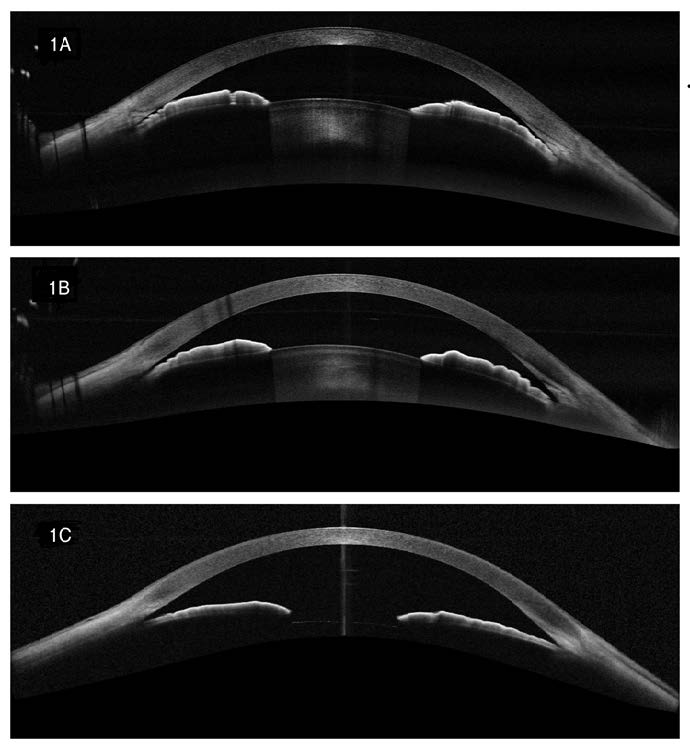 Figure 1. A: Narrow angle with iridotrabecular contact; B: Post-laser peripheral iridotomy showing minimal angleopening; C: Post cataract surgery with significant angle opening.
Figure 1. A: Narrow angle with iridotrabecular contact; B: Post-laser peripheral iridotomy showing minimal angleopening; C: Post cataract surgery with significant angle opening.
Case 2: Pigment Dispersion Syndrome with Reverse Pupillary Block
A 67-year-old white male with mild cataracts and moderate pigmentary glaucoma was progressing as determined by fields and nerve OCT with IOPs in the low 20s, despite topical usage of a prostaglandin q.h.s. OU and beta blocker b.i.d. OU. Despite an open angle by gonioscopy, OCT showed significant reverse pupillary block (Figure 2). Because of the progressing glaucoma combined with the dramatic appearance on angle OCT, we are proceeding with cataract surgery + Kahook dual blade, and he is scheduled for the near future.
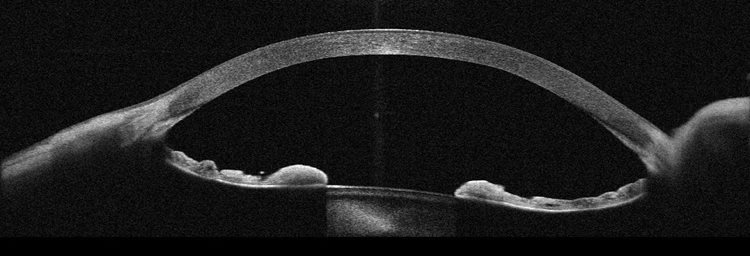 Figure 2. Reverse pupillary block in a pigmentary glaucoma patient.
Figure 2. Reverse pupillary block in a pigmentary glaucoma patient.
Case 3: Primary Angle Closure and Plateau Iris Syndrome
A 53-year-old white female came into the office to get her contact lenses updated. Her IOP, measured using iCare, was 25mm Hg OD and OS. Van Herick was graded as a 2, but the anterior chamber appeared deep centrally. Gonioscopy showed iridotrabecular contact greater than 180° with a double-hump sign. The angle OCT showed a plateau iris configuration. The optic nerves, visual fields and nerve OCTs were all unremarkable. We diagnosed her with primary angle closure with a plateau iris configuration and are proceeding with laser peripheral iridotomy.
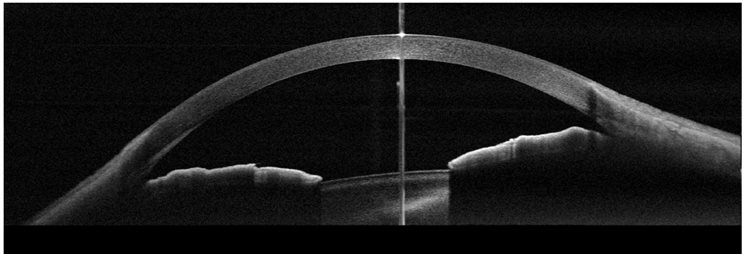 Figure 3. Plateau iris configuration.
Figure 3. Plateau iris configuration.
PACS, pigment dispersion syndrome with reverse pupillary block and plateau iris syndrome can all be clinically challenging. The ability to scan the whole anterior chamber helps to clarify these diagnoses, leading to better patient outcomes.
All FullRange® anterior segment images taken on an Optovue Solix by Visionix.
 Mike Cymbor, OD, is an ocular disease lecturer and researcher and is published in numerous journals and publications. He is a managing partner at Nittany Eye Associates in State College, PA. He is the medical director of the Glaucoma Institute of State College and a member of the Optometric Glaucoma Society and National Glaucoma Society. He is an adjunct clinical professor at the Pennsylvania College of Optometry (SALUS). He is a fellow in the American Academy of Optometry and an American Board of Optometry Diplomate. He is a Newsweek Top 175 optometrist and a PCON Top 250. He is a past "Young Optometrist of the Year" by the American Optometric Association. He received his optometric doctorate from the Pennsylvania College of Optometry (SALUS) and completed a residency at the Wilkes-Barre VA Medical Center.
Mike Cymbor, OD, is an ocular disease lecturer and researcher and is published in numerous journals and publications. He is a managing partner at Nittany Eye Associates in State College, PA. He is the medical director of the Glaucoma Institute of State College and a member of the Optometric Glaucoma Society and National Glaucoma Society. He is an adjunct clinical professor at the Pennsylvania College of Optometry (SALUS). He is a fellow in the American Academy of Optometry and an American Board of Optometry Diplomate. He is a Newsweek Top 175 optometrist and a PCON Top 250. He is a past "Young Optometrist of the Year" by the American Optometric Association. He received his optometric doctorate from the Pennsylvania College of Optometry (SALUS) and completed a residency at the Wilkes-Barre VA Medical Center.