Optical coherence tomography (OCT) is a non-invasive imaging modality that provides outstanding visualization of retinal and choroidal structure, allowing for the identification of structural abnormalities including elevations or undulations in the retinal tissue. OCT has been paramount in providing ancillary information that is not always so easy to visualize fundoscopically, such as diseases of the vitreomacular interface; in particular, vitreomacular traction (VMT). VMT is defined as attachment of the vitreous cortex to the macula within a 3 mm radius of the fovea, resulting in distortion of the foveal surface.1 VMT is a condition that is often easily overlooked on clinical exam alone.
VMT most often occurs as a result of an anomalous posterior vitreous detachment. To properly diagnose and manage VMT, the International Vitreomacular Traction Study Group (IVTS) created a classification system for VMT.2 This classification system provides a universal way of describing
this condition: First and foremost, check for the patency of the neurosensory retina. If there is a full thickness break in the retina, it is defined as a full-thickness macular hole which may have vitreous involvement. If the neurosensory retina is intact and there is evidence of VMT as defined above, then
we use the following system to classify the VMT.
The IVTS defined two main categories for diagnosis. First, to determine the size of the traction, you must utilize the line caliper or ruler on your OCT. Measuring the distance between the first attachment of the posterior hyaloid of the vitreous to the macula and the second point of attachment of the posterior hyaloid to the macula will provide the size of the traction. If the size of the traction is <1500 μm the VMT is considered focal (see Figure 1); if the size of the traction is >1500 μm the VMT is considered broad (see Figure 2). Focal VMT is often referred to as vitreofoveal traction syndrome when the traction is <500 μm in size.3
The diameter of the VMT is inversely related to prognosis. The narrower the attachment, the greater the tractional force of the vitreous on the underlying retina. Broad VMT may distribute the tractional forces over a wider expanse of the macular region. Thus, focal VMT can result in
macular hole formation or a foveolar detachment and broad VMT may result in overall thickening of the retina or epiretinal membrane formation.3
The second way to describe VMT is to look at the “company or lack of company that it keeps.” If the VMT occurs on its own without any other maculopathy, it is called isolated VMT. If the VMT occurs in the presence of another maculopathy, it is considered concurrent VMT. For example, if a patient has VMT with a choroidal neovascular membrane, it would be considered a case of concurrent VMT.
Using these classifications in conjunction with OCT can help us detect and recognize VMT in its variations when our patients present with it.
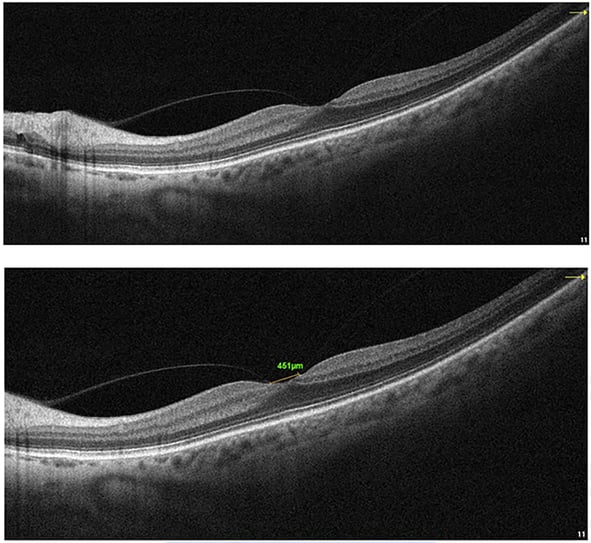 Figure 1. Focal vitreomacular traction.
Figure 1. Focal vitreomacular traction.
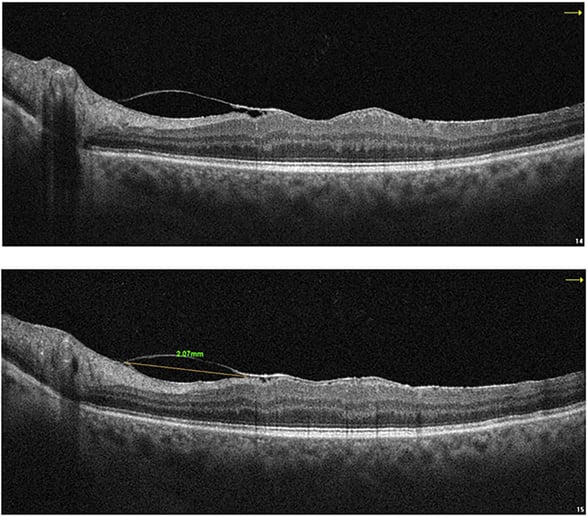
Figure 2. Broad VMT.
References:
1. García-Layana A, García-Arumí J, Ruiz-Moreno JM, Arias-Barquet L, Cabrera-López F, Figeroa MS. A review of current management of vitreomacular traction and macular hole. J Ophthalmol.
2015;2015:809640.
2. Duker JS, Kaiser PK, Binder S, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmol. 2013 Dec;120(12):2611-2619. Bottós J, Elizalde J, Rodrigues EB, Farah M, Maia M. Classifications of vitreomacular traction syndrome: diameter vs morphology. Eye (Lond). 2014 Sep;28(9):1107-1112.
 Dr. Julie Rodman is the Chief of the Broward Eye Care Institute in Fort Lauderdale, FL and a Professor of Optometry at Nova Southeastern University. Her research interests include OCT/OCT-A and Vitreoretinal Disease. Dr. Rodman has authored over thirty publications with an emphasis on retinal disease. She recently published “Optical Coherence Tomography Atlas: A Case Study Approach,” the first reference book on this topic written by an optometrist. Dr. Rodman is a member of the AOA, AAO, FOA, and ORS. She has been the recipient of numerous teaching awards and was recognized as a Primary Care Optometry News “Top 300” Optometrists and “Newsweek Best Optometrists of 2021.”
Dr. Julie Rodman is the Chief of the Broward Eye Care Institute in Fort Lauderdale, FL and a Professor of Optometry at Nova Southeastern University. Her research interests include OCT/OCT-A and Vitreoretinal Disease. Dr. Rodman has authored over thirty publications with an emphasis on retinal disease. She recently published “Optical Coherence Tomography Atlas: A Case Study Approach,” the first reference book on this topic written by an optometrist. Dr. Rodman is a member of the AOA, AAO, FOA, and ORS. She has been the recipient of numerous teaching awards and was recognized as a Primary Care Optometry News “Top 300” Optometrists and “Newsweek Best Optometrists of 2021.”
The information is intended for general informational purposes only. It is not intended as, and should not be considered, a substitute for professional medical advice, diagnosis, or treatment.
The content is not designed to replace the relationship that exists between a patient and their healthcare provider. Any medical decisions should be made in consultation with a qualified healthcare professional who can provide information tailored to your individual circumstances.
Medical procedures, case studies, and practices mentioned in this content may vary based on regional standards, local regulations, and the discretion of the providing healthcare professional. What may be considered appropriate and ethical in one country may differ in another.
The content may include general references to medical practices, medications, or treatments that are widely accepted in certain regions but may not be applicable or endorsed universally. It is important to consult with a healthcare professional in your jurisdiction to ensure the information is relevant to your specific situation.
The authors, publishers, and contributors of this content disclaim any liability for any adverse effects resulting directly or indirectly from information contained in this content. Readers should exercise their own judgment and seek the advice of healthcare professionals as appropriate.
By accessing and using this content, you acknowledge and agree to the terms of this disclaimer.