Patient description
A 31-year-old female patient has been referred to us for an opinion regarding corneal dystrophy and is experiencing increasingly frequent left eye pain. Her visual acuity is 9/10 in the right eye and 7/10 in the left eye.
Clinical Results
Upon clinical examination, we confirm the diagnosis of Granular Dystrophy Type 1. The pain is present in the morning upon waking and sometimes at night. She is experiencing recurrent corneal erosions. We propose therapeutic trans-photokeratectomy (T-PKT) as a treatment option.
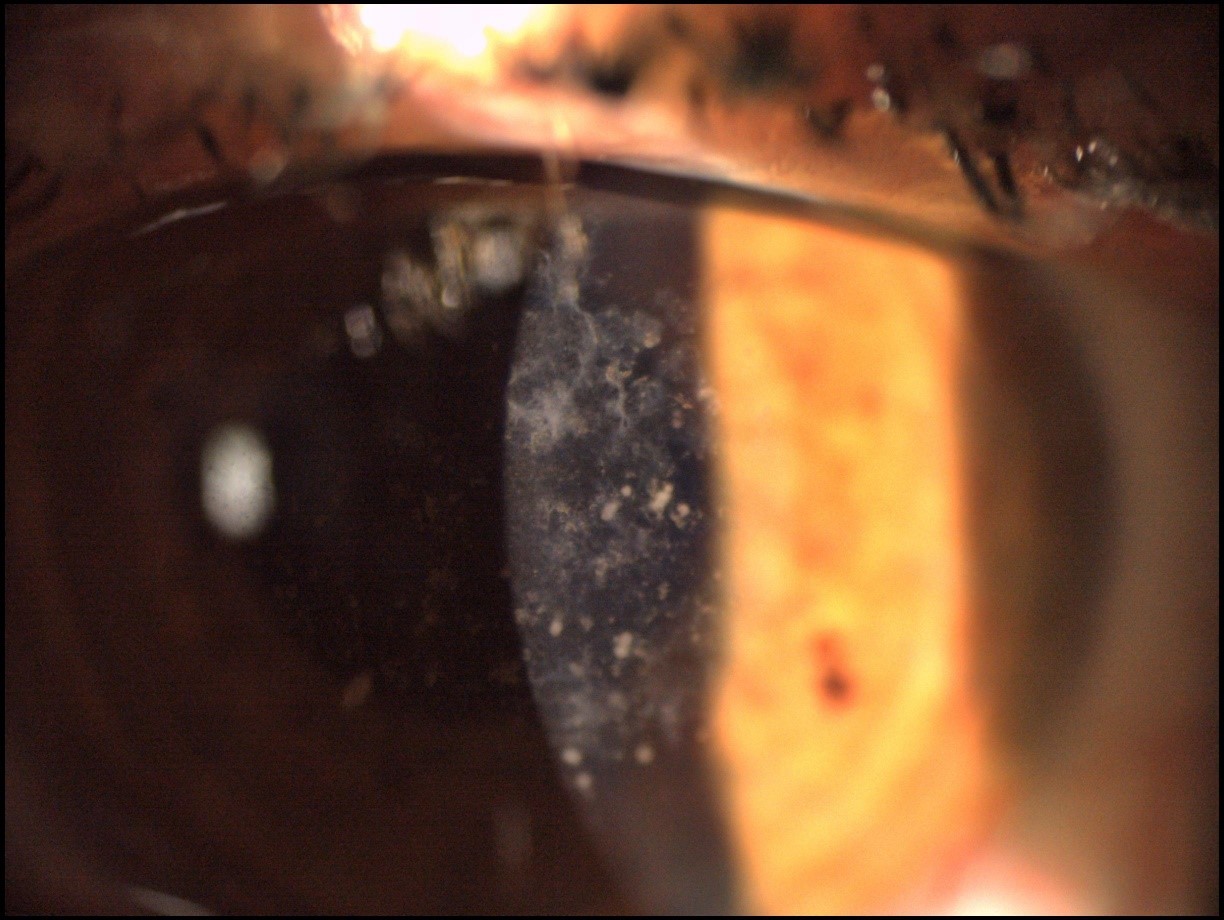
Figure 1: Slit-lamp appearance, typical of Granular Dystrophy Type 1.
%20appearance%2c%20with%20epithelial%20mapping.%20This%20clearly%20shows%20the%20irregular%20aspect%20of%20the%20subepithelial%20stroma%20and%20the%20compensation%20of%20the%20epithelium..jpg?width=1622&height=981&name=fig.%202%20Optovue%20Solix%20OCT%20(Optical%20Coherence%20Tomography)%20appearance%2c%20with%20epithelial%20mapping.%20This%20clearly%20shows%20the%20irregular%20aspect%20of%20the%20subepithelial%20stroma%20and%20the%20compensation%20of%20the%20epithelium..jpg) Figure 2: Optovue Solix OCT (Optical Coherence Tomography) appearance, with epithelial mapping. This clearly shows the irregular aspect of the subepithelial stroma and the compensation of the epithelium.
Figure 2: Optovue Solix OCT (Optical Coherence Tomography) appearance, with epithelial mapping. This clearly shows the irregular aspect of the subepithelial stroma and the compensation of the epithelium...jpg?width=1200&height=768&name=Fig.%203%20Characteristic%20appearance%20of%20Optovue%20Solix%20OCT%2c%20with%20measurement%20using%20the%20caliper.%20This%20will%20enable%20precise%20guidance%20for%20the%20Trans-PKT%20(here%2c%20a%20total%20ablation%20depth%20of%2090%CE%BC%20will%20be%20chosen)..jpg) Figure 3: Characteristic appearance of Optovue Solix OCT, with measurement using the caliper. This will enable precise guidance for the Trans-PKT (here, a total ablation depth of 90µ will be chosen).
Figure 3: Characteristic appearance of Optovue Solix OCT, with measurement using the caliper. This will enable precise guidance for the Trans-PKT (here, a total ablation depth of 90µ will be chosen).
At the 3-month postoperative follow-up, the symptoms of the left eye have significantly improved. The patient no longer experiences pain. Visual acuity has increased to 10/10.
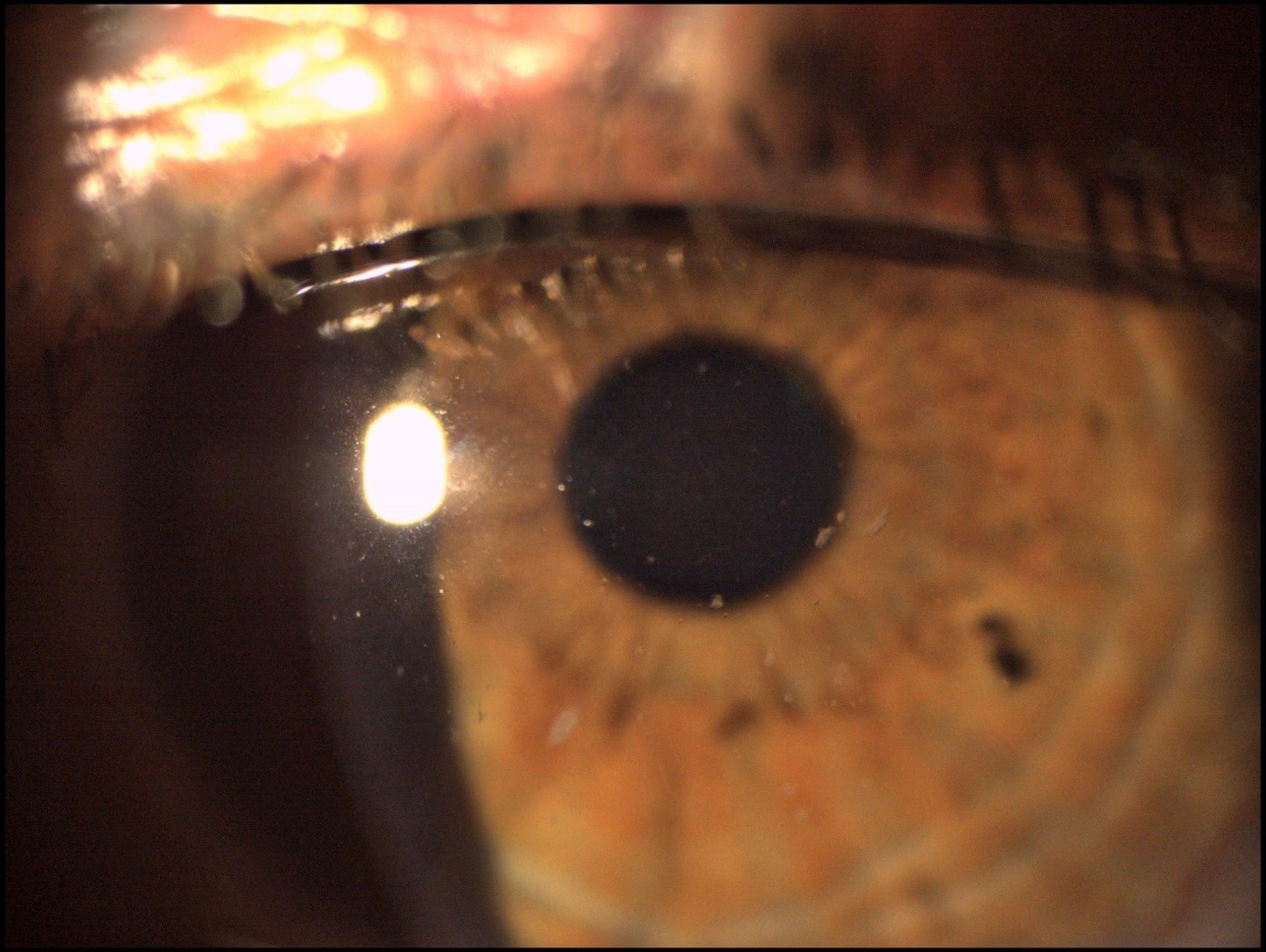 Figure 4: Postoperative slit-lamp image. Almost complete disappearance of corneal opacities.
Figure 4: Postoperative slit-lamp image. Almost complete disappearance of corneal opacities.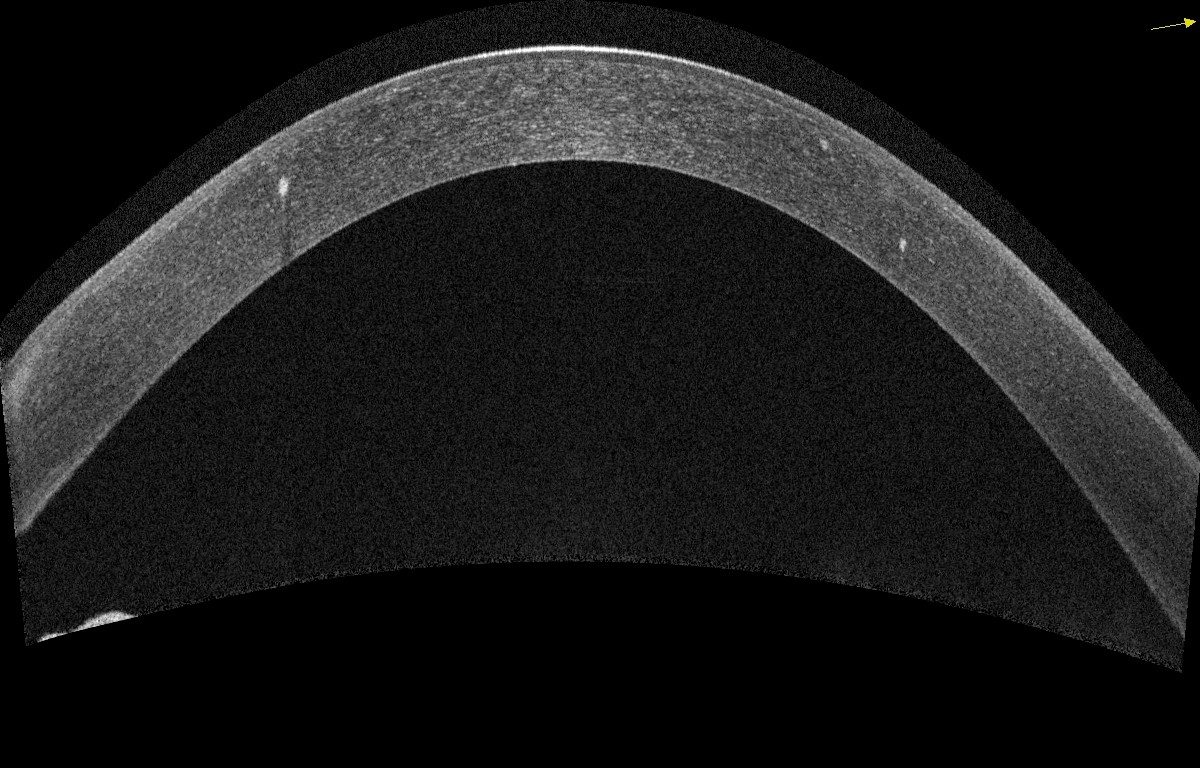
Figure 5: Postoperative appearance on Optovue Solix OCT confirming the almost complete disappearance of subepithelial opacities. Deeper opacities persist, inaccessible to therapeutic photokeratectomy.
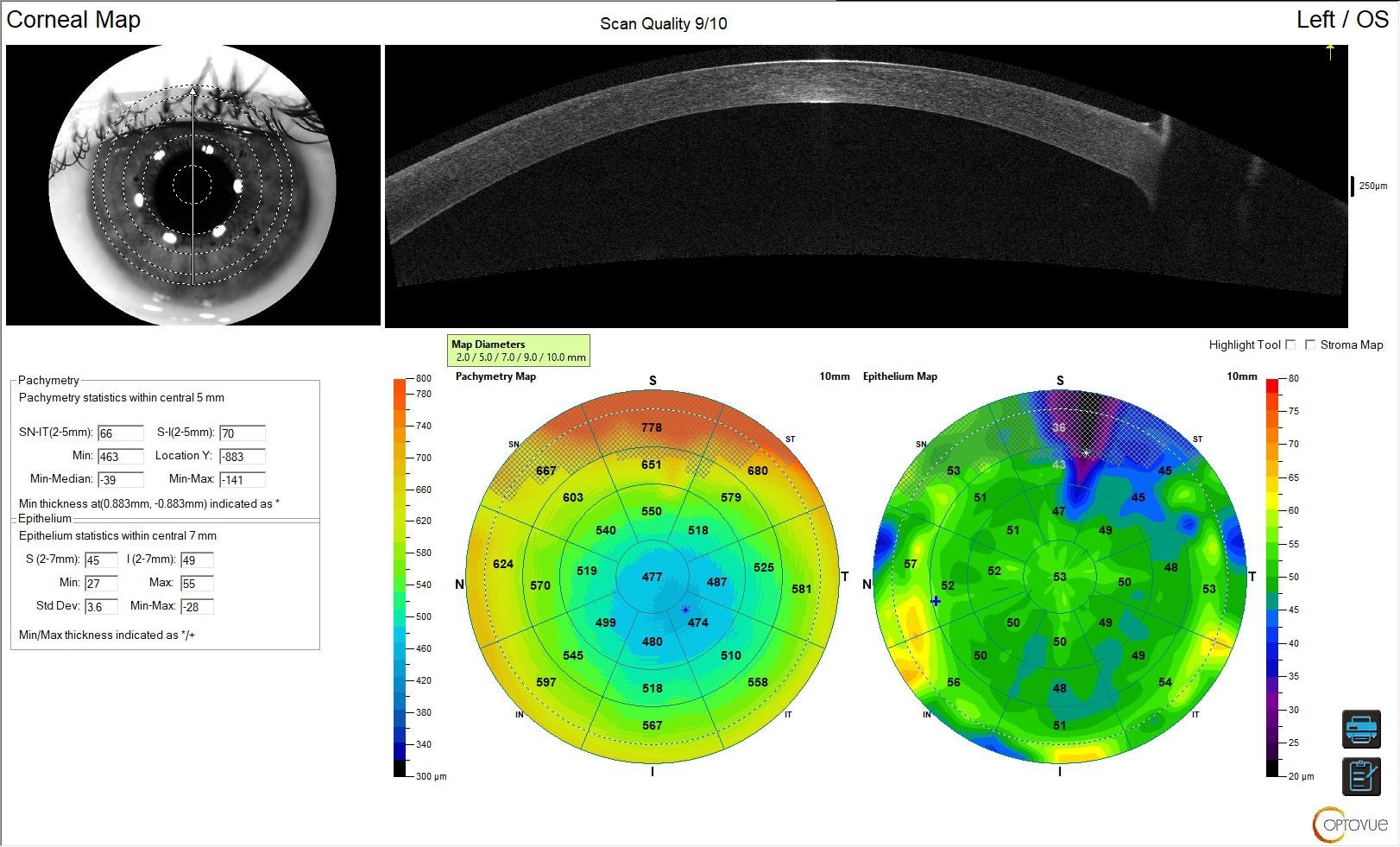 Figure 6: Epithelial mapping on Optovue Solix showing a much more regular epithelium.
Figure 6: Epithelial mapping on Optovue Solix showing a much more regular epithelium.
Conclusion
The precision of SOLIX for anterior segment OCT makes it possible to precisely guide the ablation depth of therapeutic photokeratectomy in cases of subepithelial or anterior stromal pathology.
 Dr. Dimitri Cœuru practices at the Sourdille-Atlantique Ophthalmological Institute in Saint Herblain, near Nantes. He specializes in refractive surgery, corneal surgery (particularly corneal grafts), and cataract surgery. He regularly engages with his colleagues, presenting the advantages and recommendations of new technologies in refractive surgery.
Dr. Dimitri Cœuru practices at the Sourdille-Atlantique Ophthalmological Institute in Saint Herblain, near Nantes. He specializes in refractive surgery, corneal surgery (particularly corneal grafts), and cataract surgery. He regularly engages with his colleagues, presenting the advantages and recommendations of new technologies in refractive surgery.
The information is intended for general informational purposes only. It is not intended as, and should not be considered, a substitute for professional medical advice, diagnosis, or treatment.
The content is not designed to replace the relationship that exists between a patient and their healthcare provider. Any medical decisions should be made in consultation with a qualified healthcare professional who can provide information tailored to your individual circumstances.
Medical procedures, case studies, and practices mentioned in this content may vary based on regional standards, local regulations, and the discretion of the providing healthcare professional. What may be considered appropriate and ethical in one country may differ in another.
The content may include general references to medical practices, medications, or treatments that are widely accepted in certain regions but may not be applicable or endorsed universally. It is important to consult with a healthcare professional in your jurisdiction to ensure the information is relevant to your specific situation.
The authors, publishers, and contributors of this content disclaim any liability for any adverse effects resulting directly or indirectly from information contained in this content. Readers should exercise their own judgment and seek the advice of healthcare professionals as appropriate.
By accessing and using this content, you acknowledge and agree to the terms of this disclaimer.
![[OCT Article] Granular dystrophy and therapeutic trans-photokeratectomy. Image](https://blog.visionix.com/hs-fs/hubfs/fig.1%20Slit-lamp%20appearance%2c%20typical%20of%20Granular%20Dystrophy%20Type%201..jpg?width=1250&name=fig.1%20Slit-lamp%20appearance%2c%20typical%20of%20Granular%20Dystrophy%20Type%201..jpg)